Disseminated histoplasmosis with CNS involvement
A patient progressed from diarrhea and fever to status epilepticus when infection penetrated the central nervous system (CNS).
The patient
A 28-year-old man with HIV who had been off antiretroviral therapy (ART) for six months presented with shortness of breath, diarrhea, fever, and a 20-lb weight loss over the past month. His last CD4 count, six months earlier, was 300 cells/mm3 (reference range, 500 to 1,500 cells/mm3). Since that time, he had been taking his ART only once a week. He had recently moved to Nevada from California and did not report any other travel history.

On physical exam, he had a temperature of 101.2 °F, heart rate of 128 beats/min, pulse oximetry of 84% on room air, and a respiratory rate of 40 breaths/min. Blood pressure was normal. He appeared emaciated and had labored respirations with subcostal retractions. Lungs were clear to auscultation, and neurological exam was normal. Skin findings were significant for diffuse, scattered purple papules distributed across the entire body (Figure 1). He was placed on supplemental oxygen at 40 L/min with a 100% fraction of inspired oxygen.
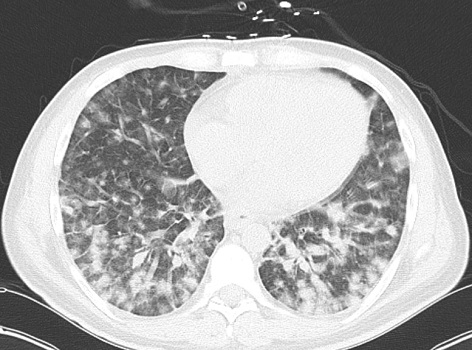
Laboratory tests revealed leukopenia of 1,200 cells/mm3 (reference range, 3,100 to 10,000 cells/mm3), CD4 count of 9 cells/mm3, CD4 percentage of 1% (reference range, 25% to 65%), HIV-1 viral load of 5.78 million copies, and a (1-3)-β-d-glucan level greater than 500 pg/mL (reference ranges, <60 pg/mL for negative, 60 to 79 pg/mL for indeterminate, and >80 pg/mL for positive). A comprehensive metabolic profile was normal, and chest CT scan showed diffuse ground-glass nodularities bilaterally, most significantly in the lower lobes (Figure 2).
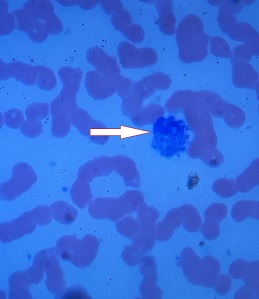
The patient was treated empirically for Pneumocystis jirovecii with trimethoprim/sulfamethoxazole and prednisone, as well as empiric vancomycin and piperacillin/tazobactam. A few days later, he developed status epilepticus requiring intubation. Fungal cultures returned positive for yeast. Histoplasma antigen and antibody testing were negative. The patient was started on fluconazole. However, a peripheral blood smear showed yeast forms inside of monocytes (Figure 3). Therapy was escalated to liposomal amphotericin and double dosing of fluconazole. The seizures could not be stopped, and the patient died seven days after admission. A skin biopsy was later found to be consistent with cutaneous histoplasmosis.
The diagnosis
The diagnosis is disseminated histoplasmosis with central nervous system (CNS) involvement. Of the invasive fungal species that cause human disease, Histoplasma capsulatum is the only species with yeast forms small enough to invade monocytes, at approximately 2 to 4 μm in length. This patient's peripheral smear was diagnostic for disseminated histoplasmosis despite the negative Histoplasma antibody testing, a relatively nonsensitive test (70% to 90%). The patient's resistant seizures are believed to be a result of CNS invasion of histoplasmosis; however, the patient's family declined a postmortem examination.

Histoplasmosis is a highly prevalent endemic fungus in the United States, with most cases occurring in the eastern U.S. near the Ohio and Mississippi Rivers and an estimated prevalence of 6 cases per 1,000 individuals in this region. There has been an increasing number of cases in individuals without travel history to these areas. While histoplasmosis was previously almost never seen in the western U.S., prevalence has now reached 2 per 1,000 individuals. Infection begins with inhalation of mold spores and transformation to yeast inside the lungs.
Disseminated histoplasmosis is a major concern for immunocompromised individuals; infection progresses to dissemination in approximately 80% of solid organ transplant recipients, and infection is fatal in approximately 30% of individuals living with HIV. Diagnosis is typically made by histoplasmosis antigen testing of urine, blood, cerebrospinal fluid, or bronchoalveolar lavage. Fungal culture is the gold standard of diagnosis; however, culture of H. capsulatum can take up to six weeks for results and thus is limited in its clinical utility. Direct visualization of yeast on a peripheral smear is highly specific, but its sensitivity is estimated to be 10%.
The Infectious Diseases Society of America (IDSA) guidelines for the treatment of moderately severe to severe progressive disseminated histoplasmosis recommend liposomal amphotericin B, 3 mg/kg daily for one to two weeks, followed by oral itraconazole, 200 mg three times daily for three days, followed by 200 mg twice daily for a total of at least a year. While CNS involvement only occurs in 5% to 10% of cases of disseminated disease, it carries high mortality, ranging from 20% to 45%. One major challenge of treatment is that amphotericin and itraconazole, the first-line antifungals for systemic histoplasmosis, have very poor CNS penetration. Fluconazole has adequate CNS penetration but poor activity against H. capsulatum. When CNS involvement is suspected, the IDSA recommends increasing the dose of liposomal amphotericin B to 5 mg/kg daily and increasing the duration to four to six weeks.
Pearls
- The presence of yeast forms smaller than leukocytes on peripheral smear is pathognomonic for histoplasmosis, even with negative Histoplasma antigen/antibody testing.
- Prompt diagnosis of disseminated histoplasmosis is vital in cases of CNS involvement, as the most effective antifungals have poor CNS penetration.



