Superior vena cava occlusion without malignancy
A patient with end-stage renal disease presented with one week of facial and left-arm edema.
The patient
A 55-year-old woman with end-stage renal disease presented with one week of facial and left-arm edema, as well as associated left-arm erythema and tenderness. She had been on hemodialysis for 20 months before presentation and had three tunneled internal jugular central line placements during that period. Four months before presentation, she had a left arteriovenous radiobasilic fistula placed, but it thrombosed. A brachioaxillary graft was placed 14 days before presentation. She had no history of malignancies, autoimmune disorder, constrictive pericarditis, aortic aneurysm, or exposure to radiation.

The patient was not in distress and was afebrile. Her blood pressure was 132/77 mm Hg, her pulse was 96 beats/min, her respiratory rate was 18 breaths/min, and her oxygen saturation was 98% on room air. She had moderate edema of the face, neck, and left upper limb. There was facial plethora as well as discrete erythema over the chest and left arm. The superficial veins of the neck and upper chest were engorged. Mild tenderness was noted on palpation of the edematous areas. A palpable thrill was present on the medial aspect of the left arm. The surgical wound on the left arm was closed and had no purulent secretion. Her laboratory values were within the expected range for a patient on hemodialysis.


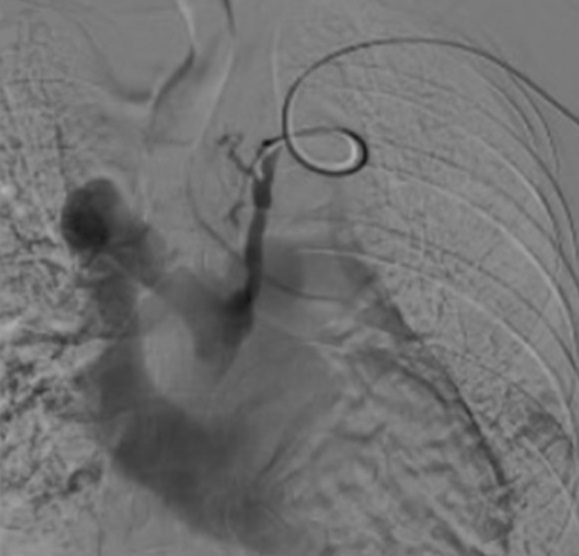
A chest CT angiogram showed superior vena cava (SVC) and left brachiocephalic vein occlusions with extensive collateral venous circulation (Figure 1). Upper-extremity venous angiography demonstrated a patent brachioaxillary graft with a network of collaterals around the shoulder, consistent with complete occlusion of the left subclavian vein (Figure 2). A large mediastinal collateral vein connected the venous drainage of the left arm with the SVC (Figure 3). An SVC venogram from the groin demonstrated complete occlusion of the SVC and no visualization of either innominate vein. The patient did not have clinical or radiological evidence of an underlying malignancy. The patient was managed conservatively (elevation of head to decrease plethora), and she tolerated dialysis through her brachioaxillary graft.
The diagnosis
The diagnosis is superior vena cava and left brachiocephalic vein occlusion. Around 15,000 SVC occlusions occur in the United States every year. For most of the 20th century, SVC syndrome was caused by malignancy, particularly small-cell lung cancer and non-Hodgkin lymphoma, in roughly 80% to 99% of cases. By the early 2000s, benign causes accounted for 40% of the cases while malignancies decreased to 60%. The most common benign cause is catheter-related SVC syndrome (70% of benign cases in a recent series), followed by pacemaker wires and aneurysms. Hemodialysis catheters are thought to have a higher risk of complications due to larger lumen size and longer placement duration. In a retrospective study, about 4% of patients with hemodialysis central vascular catheters over three years developed central venous stenosis. Additionally, the relative risk of SVC syndrome doubled with each additional catheter placed.
There are four pathophysiological mechanisms of SVC syndrome: direct vein injury from catheters, thrombosis, extrinsic compression, and neointimal hyperplasia secondary to hemodynamic abnormalities. Symptomatic management is the first step, with removal of the offending catheter or pacemaker wires if possible. Although no clinical guidelines on this topic exist, experts recommend anticoagulation for patients with SVC thrombosis, particularly for those undergoing an endovascular procedure such as thrombectomy or stent placement or in cases where the offending catheter cannot be removed. Endovascular stenting is the preferred surgical approach rather than saphenous vein bypass or grafting. Various clinical and radiological classifications have been proposed to aid in the diagnosis and treatment of SVC occlusion; however, none is widely used or accepted.
Pearls
- Although cancer continues to be the primary cause of SVC syndrome, central venous catheters and pacemaker leads now account for 40% of cases.
- The underlying cause determines treatment for SVC syndrome, with anticoagulation indicated when SVC syndrome is due to thrombosis, when the causative catheter cannot be removed, or when an endovascular procedure is planned.



