Rapidly progressive cerebral edema in cryptococcal meningitis
A patient previously diagnosed with an upper respiratory infection presented with fever, headache, and confusion.
The patient

A 44-year-old man with hypertension presented with one week of fever, headache, and confusion. He had been admitted three weeks prior with hypertensive urgency, at which time he was found to have low-grade fevers (maximum temperature 100.2 °F), ultimately attributed to a possible upper respiratory infection. At that time, his blood cultures, urinalysis, and chest X-ray were normal and SARS-CoV-2 testing was negative. On the current presentation, he was oriented but agitated and had a normal head CT.
Labs were significant for an elevated gamma gap of 4.6 g/dL (normal <4 g/dL). HIV testing was ordered and returned positive with a CD4 count of 29 cells/mm3 and a viral load of 80,600 copies/mL. Lumbar puncture revealed 33 cm H2O opening pressure (normal ≤20 cm), 10 cm closing pressure, and cerebrospinal fluid (CSF) positive for cryptococcal antigen. Liposomal amphotericin (3 mg/kg IV daily) and flucytosine (100 mg/kg four times daily) were initiated.
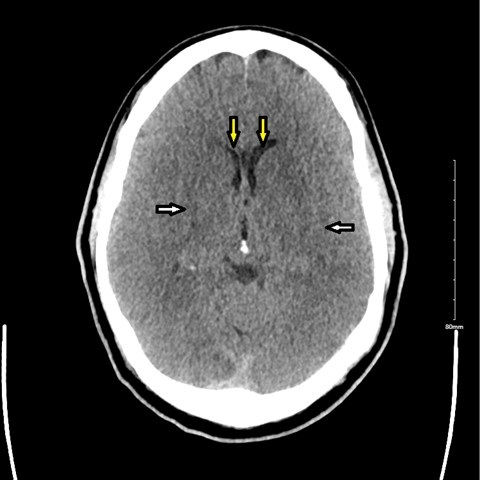
The following day, he became obtunded, requiring intubation and transfer to the ICU. A CT of the head revealed diffuse cerebral edema (Figure). He received hypertonic saline and serial lumbar punctures. A lumbar drain was not placed, due to the risk of herniation with the degree of cerebral edema. His mental status remained poor with progression to absent brainstem reflexes. His course was complicated by flucytosine-related pancytopenia and septic shock. He was eventually transitioned to comfort care and died.
The diagnosis
The diagnosis is cryptococcal meningitis in the setting of advanced HIV. Cryptococcal meningitis is a common opportunistic infection (estimated 223,100 cases worldwide per year) in patients with untreated AIDS. An important pretreatment predictor of mortality is altered mental status, defined as lethargy or obtundation. Additional predictors of poor outcomes include immunosuppressive medications and a CSF white cell count less than 20 per cubic millimeter. Cryptococcal meningitis commonly presents with headache and fever developing over a median of two weeks, with classic meningeal symptoms occurring in only 25% of patients. CT head findings are often normal or nonspecific. Diagnosis is made with serum or CSF cryptococcal antigen or CSF culture.
Cryptococcal meningitis is treated with induction therapy with liposomal amphotericin B and flucytosine for at least two weeks, followed by eight weeks of consolidation therapy with fluconazole, then fluconazole maintenance therapy for at least one year. Close neurologic monitoring and control of intracranial pressure to reduce opening pressure to less than 20 cm are critical to decrease mortality and are accomplished via serial lumbar punctures or lumbar/ventricular drains. One study found a 69% relative risk reduction in mortality with therapeutic LP. The 2010 Infectious Diseases Society of America guidelines recommend against the use of corticosteroids for elevated intracranial pressure, based on a randomized study that demonstrated no mortality benefit and increased adverse events and disability. Antiretroviral therapy is typically started at least two weeks after initiation of antifungal therapy to reduce the risk of immune reconstitution inflammatory syndrome, the incidence of which ranges from 7.6% to 30%, dependent on various factors including immune status and disease burden.
Pearls
- An elevated gamma gap, while classically associated with monoclonal gammopathy, can also be associated with chronic infections such as HIV.
- Treatment for cryptococcal meningitis consists of amphotericin and flucytosine for induction therapy, as well as serial lumbar punctures to reduce opening pressure to less than 20 cm CSF.



