Bartonella quintana endocarditis presenting as heart failure
A patient with a recent history of drinking one liter of vodka daily presented with fatigue and rash.
The patient
A 39-year-old man with a history of recent homelessness and severe alcohol use disorder, including a recent history of drinking one liter of vodka daily for a week, presented with fatigue and rash that had begun four days earlier. Temperature was 37.1 °C, blood pressure was 106/68 mm Hg, heart rate was 110 beats/min, and pulse oximetry was 96% on room air. The physical exam was significant for a 4/6 diastolic murmur at the left sternal border, pitting edema, and a nonpalpable nonblanching petechial rash of the bilateral lower extremities to the thighs, sparing the soles. The rash was not associated with nodular or tender lesions typical of Osler nodes. There were scattered splinter hemorrhages of the fingernails. The patient had no known prior valvular disease or history of heart failure.
Laboratory studies revealed microcytic anemia with a hemoglobin level of 4.3 g/dL (reference range, 13 to 18 g/dL) and a brain natriuretic peptide level greater than 4,500 pg/mL (reference range, <100 pg/mL). Iron studies revealed an iron level of 12 μg/dL (reference range, 35 to 150 μg/dL), a total iron-binding capacity of 283 μg/dL (reference range, 270 to 460 μg/dL), and a ferritin level of 15 ng/mL (reference range, 24 to 250 ng/mL). The patient's vitamin B12 level was 227 pg/mL (reference range, 180 to 914 pg/mL) and his folate level was 12.5 ng/mL (reference range, >5.8 ng/mL). The patient underwent upper GI endoscopy and colonoscopy, which were negative for a source of bleeding.
Creatinine level was 2.5 mg/dL (reference range, 0.74 to 1.35 mg/dL) and blood urea nitrogen level was 39 mg/dL (reference range, 8 to 24 mg/dL), indicating intrinsic acute kidney injury. No baseline creatinine level was available. Urinalysis revealed cloudy urine with +1 leukocyte esterase, +3 blood, and +3 protein. Microscopy showed 36 to 50 × 106/L red blood cells and 20 to 35 × 106/L white blood cells. Complement levels were low, with a C3 of 27 mg/dL (reference range, 78 to 175 mg/dL) and a C4 of 2 mg/dL (12.9 to 39.2 mg/dL).

Testing for antibodies, including anti-dsDNA, anti-ANCA, anti-MPO, and anti-PR3, was negative. Hepatitis serologies were negative. Initial blood cultures grew Staphylococcus epidermidis and Staphylococcus hominis in three out of four bottles. Empiric treatment for bacterial endocarditis was initiated (ceftriaxone, 2 g IV daily, and vancomycin, 750 mg IV twice daily), and repeat cultures the following day were negative. A chest X-ray showed cardiomegaly (Figure 1).
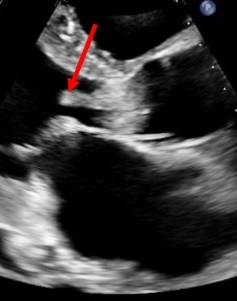
Transthoracic echocardiography revealed multiple mobile echodensities suggestive of vegetations on the aortic and mitral valve, the largest of which was 2.4 × 0.6 cm on the aortic valve (Figure 2). Aortic and mitral regurgitation were also present, and the left ventricular ejection fraction was 35%. Intraoperative transesophageal echocardiography confirmed these findings.
The patient underwent surgical resection of the vegetations and replacement of the aortic valve four days into empiric antibiotic therapy. Operative tissue showed fibrinous degeneration and acute inflammation with bacteria that were negative on Gram and acid-fast bacilli staining. Valvular tissue culture was negative. There was high suspicion for culture-negative endocarditis with contaminated initial blood cultures. The specimen was sent for broad-spectrum 16s rRNA bacterial polymerase chain reaction testing, which grew Bartonella quintana four weeks into empiric treatment. Serum Bartonella IgG titers at the time of diagnosis were 1:1,024 (diagnostic reference range, >1:800). Targeted therapy with oral doxycycline, 100 mg for three months, and rifampin, 300 mg twice daily for six weeks, was then added to the antibiotic regimen.
The diagnosis
The diagnosis is acute decompensated heart failure with reduced ejection fraction secondary to culture-negative Bartonella quintana endocarditis. Bartonella quintana is a louse-borne bacterium that is particularly common in settings of poor sanitation and alcohol misuse. Other risk factors for Bartonella endocarditis include previous valvular disease and HIV infection.
A systematic review of case studies from 40 countries showed that B. quintana causes up to 28% of culture-negative endocarditis and requires strong clinical suspicion for diagnosis. Symptoms of acute decompensated heart failure were present in almost 42% of cases, and embolization, most commonly to the spleen and brain, was present in 25.7% of cases. Diagnosis is confirmed with Bartonella IgG titers greater than 1:800.
While multivalvular involvement is less common, it has been shown to pose increased mortality risk when compared to single-valve Bartonella endocarditis. In this patient, the size of the valvular lesions suggests that subacute endocarditis was evolving over the course of weeks, devolving into acute decompensated heart failure secondary to recent binge drinking. Heavy alcohol use in endocarditis has been shown as an independent risk factor for heart failure, likely due to lower myocardial function and alcoholic cardiomyopathy.
Pearls
- Subacute infective endocarditis should be considered in patients with no cardiac history who present in acute decompensated heart failure.
- Social risk factors should prompt investigation for Bartonella quintana infection in patients with suspected infective endocarditis.



