Cases from the Medical College of Wisconsin
Endocarditis, blastomycosis, choledocholithiasis, and more.
Case 1: Endocarditis in hypertrophic obstructive cardiomyopathy
By Aileen Xu, MD, MPH, ACP Resident/Fellow Member; Mark Ehioghae, BS; and Pinky Jha, MD, MPH, FACP
The patient
A 49-year-old woman with hypertrophic obstructive cardiomyopathy, prominent systolic anterior motion of the mitral valve with associated mitral valve regurgitation, and no substance use history presented to the ED with two weeks of fatigue and worsening dyspnea on exertion. She was found to have fever (101.3 oF), tachycardia (141 beats/min), tachypnea (28 breaths/min), serum lactic acidosis (4.2 mmol/L; reference range, 0.5 to 2.0 mmol/L), and leukocytosis (white blood cell count, 14.9 × 109/L; reference range, 3.9 to 11.2 × 109/L), all consistent with sepsis. No obvious source of infection was noted on initial assessment, although she did have numerous dental caries. The physical exam was notable for a 3/6 holosystolic murmur heard best at the lower left sternal border.
The patient's symptoms improved significantly with empiric cefepime and vancomycin, along with normal saline boluses. Three days later, both peripheral blood cultures grew Gemella bergeri. Because Gemella species do not grow sufficiently to allow susceptibility testing but are historically sensitive to beta-lactams, antibiotics were narrowed to ceftriaxone.
A transthoracic echocardiogram (TTE) was notable for mitral regurgitation secondary to systolic anterior motion of the mitral valve leaflets, more severe than on a TTE from one year prior, but did not conclusively indicate endocarditis. Transesophageal echocardiogram (TEE) showed masses attached to anterior and posterior mitral valve leaflets and a perforation of the posterior valve. The patient subsequently underwent mechanical mitral valve replacement. She was discharged on six weeks total of ceftriaxone with complete resolution of symptoms.
The diagnosis
The diagnosis is subacute endocarditis related to the Gemella species in hypertrophic obstructive cardiomyopathy. Gemella bergeri is a facultative-anaerobic, catalase-negative, gram-positive cocci, part of the normal human oral, digestive, and urinary-tract flora. It was first isolated in 1998 from the blood cultures of six febrile patients, three of whom were diagnosed with subacute bacterial endocarditis. Since then, rare cases of endocarditis related to Gemella have been reported, most commonly in the mitral and aortic valves. Gemella infections in the brain, meninges, and lung have also been reported. Risk factors for endocarditis from Gemella may include male sex, congenital heart disease, valvular abnormalities, bowel surgery, and oral infection. A 2024 review of case reports found increasing incidence and antibiotic resistance in Gemella endocarditis.
In this patient, it is plausible that the anterior motion of the mitral valve and subsequent mitral regurgitation caused the valvular endothelial injury that encouraged a nidus for infection. The presence of numerous dental caries, positive blood cultures, and sepsis on presentation were suspicious for valvular seeding and prompted a thorough investigation for infectious endocarditis even following inconclusive TTE results. The sensitivities of TTE and TEE for detecting valvular vegetation are about 75% and 85% to 90%, respectively. Specificity is about 90% for either.
American College of Cardiology guidelines do not recommend therapeutic anticoagulation for hypertrophic obstructive cardiomyopathy unless the patient has clinically overt atrial fibrillation, but this patient was put on lifelong anticoagulation with warfarin due to the placement of a mechanical valve.
Pearls
- Endocarditis should be seriously considered in patients with hypertrophic obstructive cardiomyopathy and known systolic anterior motion of the mitral valve presenting with systemic infection without a clear source.
- TEE is a vital tool in detecting endocarditis, especially when TTE is inconclusive.
Case 2: Disseminated intraocular blastomycosis
By Nathan B. Rose, MD; Mitchell T. Allphin, MD; Alisha Sharma, MD, ACP Member; Kassandra E. Holzem, MD; Travis H. VandeWater, MD; and Pinky Jha, MD, MPH, FACP
The patient
A previously healthy 37-year-old man with no significant medical or ocular history presented to the ED with a 1-cm × 1-cm abscess on the left nares without any surrounding erythema after being scratched by his dog. The lesion was initially drained, and the patient was started on a 10-day course of oral amoxicillin/clavulanic acid, but the lesion persisted. Over the following two weeks, he developed pain and subjectively decreased visual acuity in his right eye, prompting another ED visit. Ophthalmology consultation revealed severe inflammation, scarring of the iris, and no view to the fundus. Ultrasound imaging confirmed inflammation and deeper involvement of the eye, together suggesting a serious intraocular infection, such as endogenous endophthalmitis or panuveitis.
An infectious cause was favored due to the elevated white blood cell count of 16.7 × 103 cells/μL (reference range, 3.9 to 11.2 × 103 cells/μL ), a concurrent suspected nasal infection, and the ophthalmologic exam findings. The patient received intraocular vancomycin and ceftazidime while undergoing an extensive workup for infectious or autoimmune causes. Laboratory testing for tuberculosis, syphilis, toxoplasmosis, HIV antibody, cat scratch disease, aspergillus, mycobacteria, viral causes, antinuclear antibodies, urine blastomycosis, histoplasmosis screens, and HLA typing for Bechet's syndrome were all negative. Blood and ocular fluid cultures, including intravitreal and anterior chamber samples, consistently showed no growth of pathogens, including herpes, varicella, or cytomegalovirus. Due to a lack of improvement, the patient underwent pars plana vitrectomy, a surgical procedure to remove the eye's internal gel, along with a biopsy and additional intravitreal antibiotics. Repeat cultures obtained intraoperatively were again negative.
Over the next month, the patient had increasing pain and further deterioration of his vision and was admitted for additional workup. The skin lesion on the left nares had a verrucous appearance, raising suspicion of an underlying fungal infection. A biopsy of the skin lesion showed broad-based budding yeast with double refractile walls consistent with blastomycosis. A CT of the chest revealed a right-sided, platelike consolidation with volume loss along the oblique and horizontal fissure that was suspicious for prior blastomycosis given the skin biopsy.
Notably, the patient had no occupational or recreational exposures to likely sources of blastomycosis. The ocular findings and nose lesion were presumed to be the result of disseminated blastomycosis. The patient was treated with amphotericin and transitioned to voriconazole for at least a year. Since he had persistent pain in his eye and no light perception, an enucleation was planned.
The diagnosis
The diagnosis is disseminated intraocular blastomycosis. Blastomycosis is a systemic pyogranulomatous infection caused by the thermally dimorphic fungus Blastomyces dermatitidis or Blastomyces gilchristii. The fungus is endemic to the midwestern, southeastern, and south-central United States between the Mississippi and Ohio Rivers. The lungs are the most common site of infection (91%), followed by the skin (18%), bones (4%), genitourinary tract (2%), and central nervous system (1%). Since a case of systemic blastomycosis involving the eyelid was first reported in 1914, fewer than 50 published works have discussed eye-related presentations. Eye complications like conjunctivitis, keratitis, or full-thickness eye infections (e.g., endophthalmitis, panophthalmitis) are rare. Prompt ophthalmological evaluation and diagnosis are crucial, as untreated or incorrectly treated intraocular infections can result in secondary glaucoma, corneal opacification, postinflammatory cataracts, retinal detachment, and total vision loss, frequently requiring enucleation. This risk is further amplified in patients with underlying conditions such as diabetes, immunosuppression, IV drug use, or indwelling catheters, which predispose patients to systemic fungal infections.
Initial treatment is typically amphotericin B, especially if the central nervous system is involved. Adjunctive intravitreal antifungal medications can also be considered. Following initial amphotericin B therapy, systemic fungal infections are typically managed with oral azoles such as voriconazole due to its high oral bioavailability (96%) and good ocular penetration. Voriconazole is also preferred for its better tolerance, particularly among patients with impaired kidney function. The recommended oral dose is 200 to 400 mg twice daily, adjusted based on therapeutic drug monitoring. Treatment typically lasts for six to 12 months, with longer durations for severe or immunocompromised cases to prevent relapse.
Pearls
- Consider fungal etiologies like blastomycosis in unexplained intraocular inflammation, especially when accompanied by systemic symptoms or refractory infections.
- In disseminated blastomycosis, thorough skin examination and early antifungal treatment are critical to facilitate diagnosis and prevent poor outcomes.
Case 3: Choledocholithiasis in hemoglobin Santa Ana
By Amen An, BS, and Pinky Jha, MD, MPH, FACP
The patient
A 19-year-old man with hemoglobin Santa Ana presented with a five-day history of right upper quadrant abdominal pain, worsening jaundice, nausea, and moderate amounts of nonbilious, nonbloody emesis. On examination, he was afebrile with blood pressure ranging from 130/70 to 150/90 mm Hg and an oxygen saturation of 86% on room air (later confirmed to be typical for the patient given his hemoglobinopathy). His body mass index was 20 kg/m2. Generalized icterus, right upper quadrant abdominal tenderness, and splenomegaly were observed.
Laboratory findings were significant for direct bilirubinemia greater than 20 mg/dL (reference range, ≤0.3 mg/dL) and a total bilirubin level of 33.7 mg/dL (reference range, 0.2 to 1.2 mg/dL). Liver enzymes revealed a cholestatic pattern of liver injury with an alanine aminotransferase level of 293 U/L (reference range, <42 U/L), an aspartate aminotransferase level of 200 U/L (reference range, <50 U/L), and an alkaline phosphatase level of 305 U/L (reference range, 40 to 129 U/L). The patient's lactate dehydrogenase level was 689 U/L; his chart indicated chronic elevations above 500 U/L (reference range, 135 to 225 U/L). There was no leukocytosis, and the hemoglobin level was 11.9 g/dL, compared to a baseline between 9 to 11 g/dL (reference range, 13.0 to 17.0 g/dL). The platelet count was 114,000 cells/µL (reference range, 150,000 to 350,000 cells/µL), and the reticulocyte count was 18.9%, compared to 22.4% five years ago during a hyperhemolysis episode (reference range, 0.5% to 2.2%). The remainder of the workup, including renal function, lipase level, hepatitis panel, and cytomegalovirus quantitative nucleic acid amplification testing, was unremarkable.
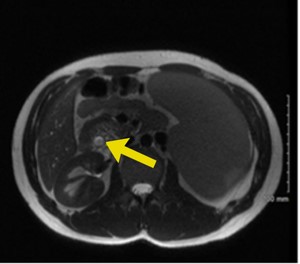
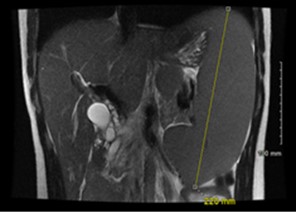
Right upper quadrant ultrasound revealed a distended gallbladder with cholelithiasis and no evidence of cholecystitis. Magnetic resonance cholangiopancreatography (MRCP) demonstrated biliary ductal dilation to 0.9 cm (reference range, 0.18 to 0.6 cm) (Figure 1), edematous pancreatitis, and splenomegaly to 22 cm (reference range, 12 to 14 cm) (Figure 2). Endoscopic retrograde cholangiopancreatography (ERCP) was notable for removal of a 5-mm pigmented stone, and laparoscopic cholecystectomy was performed without complications. Concurrent splenectomy with laparoscopic cholecystectomy was a consideration for this patient. However, given the patient's stable hemoglobin levels and recommendations that patients receive pneumonia, meningitis, and flu vaccinations at least two weeks prior to splenectomy, the procedure was deferred to be scheduled electively at outpatient follow-up.
The diagnosis
The diagnosis is choledocholithiasis. According to a 2019 guideline from the American Society for Gastrointestinal Endoscopy (ASGE), the diagnosis of choledocholithiasis involves assessing a combination of clinical symptoms (e.g., right upper quadrant or epigastric abdominal pain, nausea, vomiting), liver function test abnormalities (e.g., elevated aminotransferase, total bilirubin, and alkaline phosphatase levels), and imaging studies (e.g., endoscopic ultrasound, MRCP). This multifactorial approach is necessary because the sensitivities and specificities of each diagnostic component individually are not well established.
The ASGE recommends categorizing patients as high, intermediate, or low risk for choledocholithiasis. Factors that place patients at high risk for choledocholithiasis as opposed to an alternative intra-abdominal source of infection include any of the following: total bilirubin level above 4 mg/dL, bile duct dilation (>6 mm in patients with an intact gallbladder or >8 mm in those with previous cholecystectomy), and evidence of stones or cholangitis on imaging. Patients considered at intermediate risk are often older than 55 years of age and present with abnormal liver function tests, and/or have bile duct dilation greater than 6 mm. Patients without any of these findings are placed in the low-risk category. Low-risk patients may not require immediate intervention, but patients classified as intermediate or high risk typically undergo further evaluation with additional imaging such as MRCP and, if indicated, treatment with subsequent intervention with ERCP and/or cholecystectomy.
Choledocholithiasis most often occurs in the setting of bile stasis, which increases the likelihood of intraductal stone formation. The incidence and prevalence of choledocholithiasis in hemoglobinopathies are not well documented, but the incidence and prevalence of cholelithiasis have been investigated in sickle cell disease and beta-thalassemia. Choledocholithiasis in this case was presumed to be secondary to the patient's known hemoglobin Santa Ana, a rare and unstable hemoglobinopathy characterized by the substitution of leucine by proline at the 88th position of the beta-globin chain. This alteration results in the precipitation of hemoglobin and can present similarly to other hemoglobinopathies, with symptoms including chronic hemolytic anemia, gallstones, jaundice, and splenomegaly.
Pearls
- Hemoglobin Santa Ana is a rare and unstable hemoglobinopathy that can present clinically with chronic hemolytic anemia, gallstones, jaundice, and splenomegaly.
- Vaccinations for encapsulated organisms are recommended prior to splenectomy due to increased risk for infection.
Case 4: Tetanus
By Emily Wendel, BS, and Hayley Vandenboom, MD, ACP Resident/Fellow Member
The patient
A 36-year-old man presented to the ED with one day of muscle spasms. The spasms began in the right hamstring and progressed to his left gastrocnemius and right muscles of mastication. The patient reported sustaining a scrape from a piece of metal protruding from a concrete post at his job as a bus driver five days prior to symptom onset. He stated he removed rust from the open wound, and though there was mild, brief bleeding, the wound otherwise healed quickly without erythema or purulence and was unremarkable on presentation. His last documented Tdap vaccination had been 18 years prior to the injury.
Examination revealed vital signs within normal limits, with no fever, diaphoresis, or indications of autonomic instability to raise concern for systemic infection. Initial laboratory workup, including creatine phosphokinase level, a complete blood count, and a complete metabolic panel, was unremarkable. The patient had a slightly elevated white blood cell count of 11,400 cells/µL (reference range, 4,000 to 11,000 cells/µL).
Tetanus immunoglobulin, tetanus toxoid, and IV metronidazole were administered. Symptom control with IV diazepam was initiated due to progressive muscle spasms and concern for progression to laryngospasm-induced airway compromise. The patient was reporting sensations of airway constriction and increased work of breathing. However, increasing doses of diazepam led to concerns of oversedation. Magnesium sulfate infusion was initiated as an adjunct therapy (40 mg/kg bolus followed by 2 g/h) but resulted in vascular occlusion, observed in a superficial vein used for its administration, necessitating discontinuation. By hospital day eight, the patient began to report subjective symptom improvement. A benzodiazepine taper was initiated, with 50% reduction in diazepam on the ninth day of admission. By day 16 of hospitalization, the patient no longer required benzodiazepine for symptom control and was managed with acetaminophen, lidocaine patches, and physical therapy. The patient was discharged home on hospital day 16, although he noted continued muscle soreness that was expected to persist for several weeks.
The diagnosis
The diagnosis is generalized tetanus. Generalized tetanus accounts for 80% of incident cases of tetanus and is characterized by generalized rigidity and spasms. Localized tetanus presents with spasms restricted to the site of injury and accounts for 2% of cases, while cephalic tetanus presents with neurologic symptoms and represents fewer than 1% of cases. The diagnosis relied on clinical signs and history due to the rarity of tetanus in developed regions and the absence of confirmatory laboratory tests.
Tetanus infection occurs secondary to wound inoculation with Clostridium tetani, a spore-forming obligate anaerobic bacteria found in soil and within the intestinal tracts of animals and humans. When spore germination occurs at the wound site, it may lead to the release of tetanospasmin and tetanolysin into the bloodstream, resulting in damage to neuromuscular endplates of inhibitory neurons via the process of retrograde axonal transport. Tetanospasmin is a neurotoxin that causes muscle spasms, while tetanolysin causes tissue damage. The toxins act by preventing the release of inhibitory neurotransmitters causing unopposed muscle stimulation, hypertonia, and spasms. The incubation period can vary broadly but generally ranges from three to 21 days with an average of eight days. A shorter incubation period has been associated with a more severe prognosis and course of illness. Full recovery can take months due to the neurotoxic effects requiring axon regeneration for complete symptom resolution.
Tetanus is an increasingly rare diagnosis in the developed world thanks to vaccination campaigns and prophylactic treatments in patients sustaining high-risk wounds, with only 29 cases on average per year in the United States from 2009 to 2018. In high-resource settings, risk factors besides being unvaccinated include immunocompromised status, diabetes with infected ulcers, IV drug use, dental infections, and poorly sanitized burns.
Given the low prevalence of tetanus cases in high-resource settings and the lack of confirmatory laboratory testing, it is important to consider a broad differential in patients with presentations including electrolyte imbalances and seizures or other neuropsychological symptoms. Additionally, this report is a reminder to advocate for appropriate administration of a Tdap booster every 10 years, even in younger patients without significant comorbidities.
Pearls
- Balancing effective spasm control using benzodiazepines while avoiding oversedation and airway compromise is crucial in tetanus management.
- Educate patients about the importance of tetanus vaccination and wound care to prevent tetanus infection, especially in regions with declining vaccination rates.
